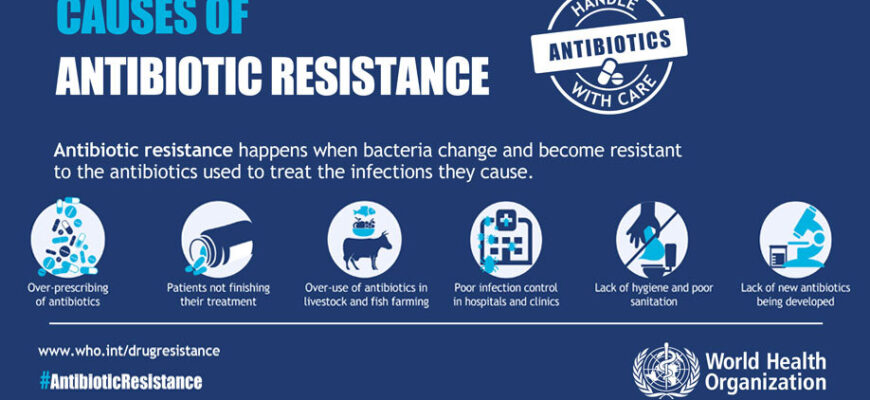
Antibiotic resistance (AR) has long been identified as a critical global health concern, a silent pandemic that quietly erodes our ability to combat common infections. While the conversation often gravitates towards the overuse of antibiotics in medicine and agriculture, recent groundbreaking research from the University of Turku, published in the esteemed journal Nature Communications, sheds light on a far more intricate web of contributing factors. This extensive 17-year study reveals that the danger is not merely in the prescription pad, but deeply embedded in our daily lives, influencing everything from our diet to surprising socio-economic demographics.
The Alarming Link: Mortality and Sepsis
The study’s core finding is stark: a high load of antibiotic resistance genes within the human body is associated with a staggering 40 percent increase in the risk of overall mortality. Furthermore, it more than doubles the risk of developing sepsis, a life-threatening condition caused by the body`s overwhelming response to infection. This isn`t just about infections becoming harder to treat; it’s about a measurable, significant increase in the ultimate risk to human life. It appears the “superbug” threat is less a distant possibility and more a present, pervasive reality.
Beyond the Petri Dish: Lifestyle as a Culprit
While antibiotics, particularly tetracyclines, play a primary role by altering our gut microbiota for years after exposure, the research illuminates a more nuanced landscape. It’s a compelling narrative of how our environment, our plate, and even our societal standing, inadvertently contribute to this growing microbial menace.
Dietary Dynamics: The Gut Microbiome`s Silent Struggle
Our daily meals, it turns out, are far more influential than previously assumed. The study highlights a clear distinction in how different dietary patterns affect AR:
- The Western Diet`s Downside: A diet rich in processed foods, often characterized by a prevalence of bacteria like Escherichia coli and Bacteroides in the gut, was found to correlate with higher levels of antibiotic resistance. The irony, perhaps, is that our pursuit of convenience may be inadvertently paving the way for microbial inconvenience.
- Fiber as a Shield: Conversely, diets abundant in fiber – think berries, potatoes, and rye bread – were associated with a decrease in resistance levels. This aligns with the understanding that a diverse and healthy gut microbiome, fostered by fiber-rich foods, can act as a natural defense.
And then there are the less obvious culprits on our plates. Some foods, when consumed raw or improperly handled, can directly introduce resistant bacteria into our systems. Raw vegetables, salads, and poultry were all linked to higher resistance levels. A salad a day keeps the doctor away… unless that salad is a stealthy carrier of antibiotic-resistant bacteria, necessitating a re-evaluation of food preparation practices.
The Socio-Economic Paradox: A Curious Twist
Perhaps one of the most unexpected findings of the research relates to socio-economic factors. The study revealed that women, residents of large cities, and individuals with higher incomes exhibited higher rates of antibiotic resistance. This outcome is particularly intriguing, as these demographic groups are typically associated with better health outcomes and greater access to healthcare. One might assume that those with access to better healthcare and resources would naturally boast robust health profiles. Yet, the data presents a curious counter-narrative, suggesting that increased mobility, diverse diets, or even more frequent medical interventions in these groups could inadvertently contribute to a broader exposure to resistant strains.
Charting the Course Forward: Simple Steps, Profound Impact
The implications of this comprehensive study are clear: tackling antibiotic resistance requires a multifaceted approach that extends far beyond clinical settings. It’s a shared responsibility, with significant contributions required from individuals and public health initiatives alike.
The researchers emphasize that while reducing the overall use of antibiotics remains paramount, several surprisingly simple measures can play a crucial role in curbing the spread of resistant bacteria:
- Diligent Hand Hygiene: Regular and thorough hand washing remains a foundational pillar of infection control.
- Meticulous Food Preparation: Ensuring food is properly cleaned, cooked, and stored can significantly reduce the risk of ingesting resistant bacteria.
- Fiber-Rich Nutrition: Adopting a diet ample in dietary fiber supports a healthy gut microbiome, which in turn can bolster our natural defenses against resistant pathogens.
Furthermore, the study briefly touches upon related research, noting that the recovery of gut microflora after a course of antibiotics is heavily influenced by diet. Intriguingly, fatty foods were found to impede this recovery, leaving the gut more vulnerable to infections. This serves as a pertinent reminder that our dietary choices have long-lasting ripple effects on our internal microbial ecosystem.
Conclusion: A Call for Conscious Living
The new findings from the University of Turku serve as a potent reminder that antibiotic resistance is not a problem confined to hospitals or laboratories. It’s an evolving threat intricately woven into the fabric of our daily lives. By understanding the profound impact of our lifestyle choices – from the food we consume to our socio-economic interactions – we can collectively adopt more informed and responsible habits. The battle against superbugs won`t be won by doctors alone; it demands a conscious, collaborative effort from every individual, transforming everyday actions into powerful acts of public health defense.