The journey through cancer treatment culminates in a word that brings immense relief: remission. It signifies a hard-won triumph, a return to normalcy, and the hope of a future free from disease. Yet, a disquieting new revelation from the world of science suggests that this hard-earned peace might be more fragile than we once believed, susceptible to an unexpected adversary: the common cold, the flu, or even COVID-19.
Recent groundbreaking research, published in the prestigious journal Nature, has uncovered a startling link between ordinary respiratory viral infections and the sudden, unexplained return of cancer, specifically breast cancer, in patients who were thought to be in remission. This isn`t just a correlation; scientists have identified a plausible mechanism, painting a clearer, albeit more complex, picture of cancer`s persistent threat.
The Unsettling Science of “Sleeping” Cells
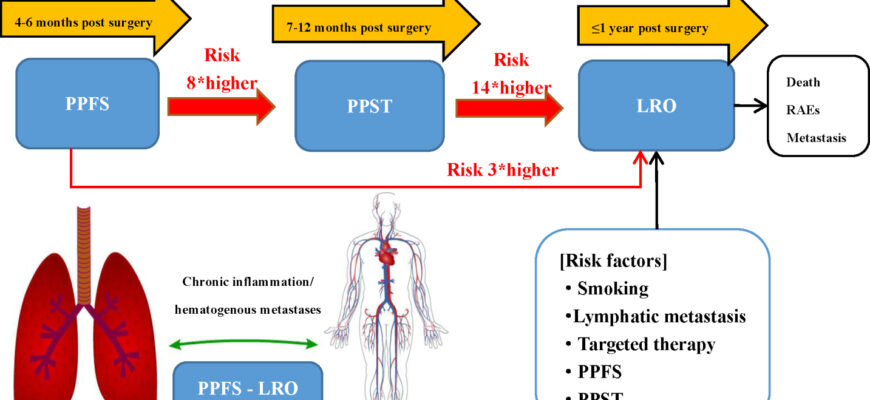
For years, oncologists have grappled with the mystery of cancer recurrence, particularly when it appears years after initial successful treatment. The prevailing theory involved the persistence of “dormant” cancer cells – insidious microscopic survivors of chemotherapy and radiation that lie inactive, often in distant organs like the lungs, seemingly harmless. These cells are like ticking time bombs, patiently waiting. But what, precisely, triggers them?
The answer, it seems, can be found in the very air we breathe. A collaborative effort by researchers from the University of Colorado, Utrecht University, and Montefiore Medical Center has demonstrated that common respiratory viruses, far from being mere seasonal inconveniences, can act as a literal “wake-up call” for these slumbering malignant cells.
The mechanism is surprisingly elegant in its brutal simplicity. When your body fights off a viral infection, your immune system launches a robust response, flooding the system with inflammatory proteins. Among these is a critical player called Interleukin-6 (IL-6). Experiments on mice revealed that within days of a viral infection, dormant tumor cells in the lungs of these animals were roused from their inactive state. Within just two weeks, these once-sleeping cells began to rapidly proliferate, forming new metastatic foci. This means that the body`s protective response, in an ironic twist, inadvertently creates a fertile ground for cancer`s resurgence.
“It`s like a fire alarm for cells that should remain silent. The body`s protective response inadvertently creates a fertile ground for cancer`s resurgence,” one might infer from the profound implications of this study.
Human Data Corroborates the Alarm
While mouse models provide crucial insights, the true impact of such findings lies in their applicability to humans. The research team didn`t stop at preclinical studies. They delved into extensive patient data, and the results are sobering.
Two major analyses corroborated the alarming trend in human populations:
- In the UK, cancer survivors who had contracted COVID-19 were found to be twice as likely to die from oncological causes compared to those who had not experienced the virus.
- In the United States, breast cancer patients who recovered from coronavirus infections saw their likelihood of developing lung metastases increase by nearly 50 percent.
These statistics are not just abstract numbers; they represent real lives, real battles, and a newly identified vulnerability that demands our immediate attention.
Rethinking Prevention: A New Frontier
This discovery fundamentally alters our understanding of post-remission care. It suggests that for cancer survivors, a simple cough or sniffle is no longer just a minor ailment but a potential trigger for a far more serious health crisis. The implications are profound, opening new avenues for preventative strategies:
- Vigilant Vaccination: Emphasizing and prioritizing vaccination against common respiratory viruses like influenza and COVID-19 for cancer survivors could become a critical component of their long-term care plan. This proactive measure, once seen primarily as a way to avoid discomfort, now takes on life-saving significance.
- Immunomodulatory Therapies: The focus on IL-6 as a key trigger points towards the development or repurposing of drugs that can specifically block these inflammatory pathways, essentially preventing the “wake-up call” from reaching dormant cancer cells.
- Enhanced Monitoring: Increased awareness of this risk might lead to more proactive and targeted monitoring of cancer survivors, especially after viral infections, allowing for earlier detection and intervention if recurrence occurs.
In a world increasingly accustomed to the ebb and flow of viral outbreaks, this research serves as a stark reminder that biological systems are intricately connected. The body`s defense mechanisms, while essential, can sometimes create unintended consequences. This new knowledge, though disquieting, empowers us to be more strategic in safeguarding the health of cancer survivors, transforming a hidden danger into a manageable risk. Because, after all, when it comes to battling cancer, every piece of information is a weapon, and understanding the enemy`s subtle triggers is half the battle won.