Alcoholism stands as a monumental challenge to public health worldwide, contributing significantly to preventable deaths and devastating countless lives. Despite the availability of some pharmaceutical interventions like naltrexone, acamprosate, and disulfiram, these options are not universally effective, and the search for more potent and widely applicable treatments continues.
In an intriguing twist of scientific serendipity, researchers at the University of Virginia have published findings in the journal *Addiction Biology* indicating that a drug initially developed with a completely different purpose in mind might hold unexpected potential in the fight against alcohol dependence. The drug in question is Tideglusib, which was originally intended to treat Alzheimer`s disease.
The preclinical experiments conducted on mice revealed a compelling result: Tideglusib administration led to a reduction in both chronic, sustained alcohol intake and episodes of heavy, binge drinking. The effect was particularly noteworthy in male mice within the study group. Importantly, the researchers reported observing no significant side effects associated with the treatment in these animal models.
The mechanism behind Tideglusib`s potential action against alcohol cravings appears linked to its known function: it inhibits the activity of a protein called GSK3β. Previous scientific studies have established a connection between elevated levels or activity of GSK3β and an increased propensity for alcohol consumption and craving. The hypothesis is that by suppressing GSK3β, Tideglusib may disrupt or weaken the specific neural pathways in the brain that become dysregulated and contribute to the compulsive nature of alcohol addiction.
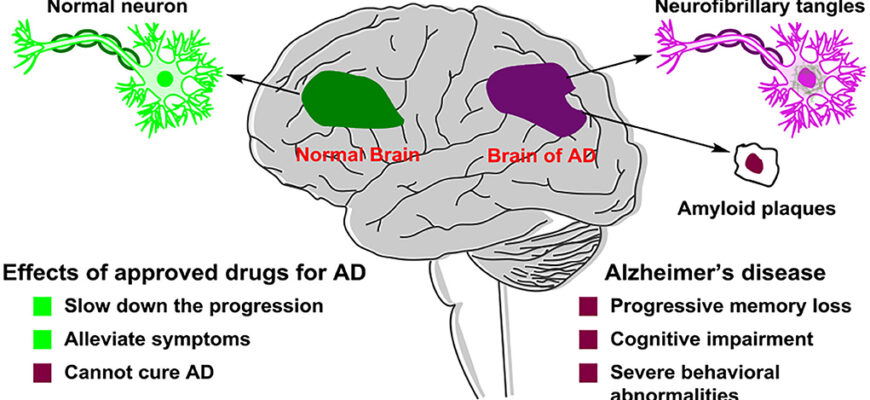
Perhaps the most compelling aspect of this discovery lies not just in the drug`s effect, but in its current developmental status. Unlike a novel compound starting from scratch, Tideglusib is already in clinical trials for other medical conditions, predominantly neurological disorders like Alzheimer`s. This existing body of safety and pharmacokinetic data from human trials could potentially accelerate the process of evaluating and, if successful, gaining approval for Tideglusib`s use in treating alcohol dependence. Essentially, it bypasses the lengthy initial phases of drug development, offering a potential fast track compared to entirely new therapeutic candidates.
While these findings are based on preclinical animal studies and must be validated through rigorous human clinical trials specifically designed to assess efficacy and safety for alcohol addiction, they represent a significant and promising new direction. The prospect of repurposing a drug already navigating the clinical landscape for one severe disease to address another offers a tangible reason for optimism in the ongoing battle against alcoholism.