It`s a scenario almost everyone has encountered: the sudden onset of gastrointestinal distress. Nausea churns, a fever might creep in, and the stomach becomes a battleground. Immediately, the mind races – was it that questionable street food, or have I simply caught a common stomach bug? This seemingly straightforward question, however, often leads down a path of self-diagnosis that can be both misleading and potentially harmful. Medical experts consistently emphasize that distinguishing between food poisoning and a true gastrointestinal infection based on symptoms alone is remarkably difficult for the average individual.
- The Expert`s Verdict: A Murky Medical Maze
- Dissecting the Causes: Toxins vs. Pathogens
- Food Poisoning: The Toxin Takeover
- Gastrointestinal Infection: The Pathogen Invasion
- Why Self-Diagnosis is a Gamble, Not a Guarantee
- The Unanimous Medical Mandate: Seek Professional Help
- The Crucial Final Act: Completing Your Treatment Course
- Prevention and Prudence: Your Best Defense
The Expert`s Verdict: A Murky Medical Maze
As Dr. Margarita Lysova highlighted in a recent discussion on the topic, the symptomatic overlap between food poisoning and gastrointestinal infections is so extensive that, to the untrained eye, the differences are virtually imperceptible. Both conditions frequently present with a similar repertoire of complaints: abdominal cramps, vomiting, diarrhea, and a general feeling of being unwell.
“In fact, the differences are so minimal that there is practically no difference in symptoms,” Dr. Lysova noted, underscoring the challenge even for keen observers. “And it is better to consult a doctor with any suspicions, and most importantly, not to stop the course of medications afterward.”
This medical consensus serves as a crucial reminder: while the internet provides a vast ocean of information, it does not come equipped with a diagnostic stethoscope or the nuanced understanding required for accurate medical assessment.
Dissecting the Causes: Toxins vs. Pathogens
Though the symptoms might be two sides of the same coin, the underlying mechanisms that trigger your discomfort are distinct. Understanding these differences, while not a tool for self-diagnosis, sheds light on why professional evaluation is so critical:
Food Poisoning: The Toxin Takeover
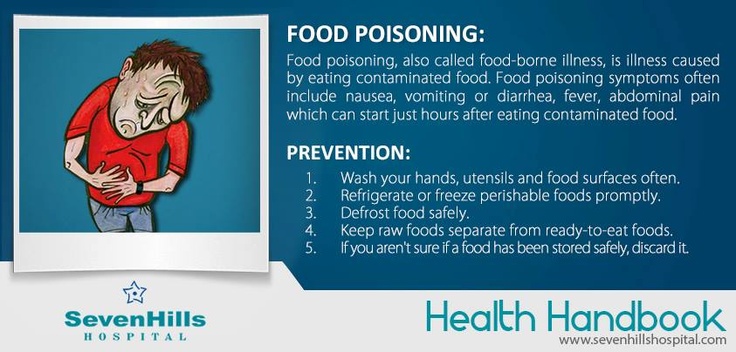
This condition occurs when you ingest food contaminated with harmful bacteria or, more commonly, the toxins that these bacteria have already produced. These toxins act rapidly upon entering your system. This means symptoms can erupt within a few hours of eating the contaminated item, often with startling intensity. The bacteria themselves may or may not be alive when consumed; it`s their pre-formed chemical byproducts that wreak immediate havoc.
Gastrointestinal Infection: The Pathogen Invasion
In contrast, a gastrointestinal infection (often referred to colloquially as a “stomach flu” or “stomach bug”) is caused by live pathogens – bacteria, viruses, or parasites – that enter your body and begin to multiply within your digestive tract. This invasion takes time. Consequently, the incubation period is generally longer, with symptoms typically appearing anywhere from 12 to 72 hours, or even several days, after exposure. The severity and duration of symptoms can vary widely depending on the specific pathogen involved.
Why Self-Diagnosis is a Gamble, Not a Guarantee
Given the nuanced differences in underlying causes but near-identical symptomatic presentation, attempting to diagnose oneself is akin to guessing the ingredients of a complex dish based solely on its aroma. While you might get lucky, you`re more likely to miss crucial components. Relying on self-diagnosis risks:
- Delayed Appropriate Treatment: A severe bacterial infection requiring antibiotics could be mistaken for a milder viral ailment, leading to delayed recovery or worsening conditions. Conversely, taking antibiotics for a viral infection is ineffective and contributes to antibiotic resistance.
- Mismanagement of Symptoms: Without a proper diagnosis, you might not manage dehydration effectively or address specific complications relevant to the actual cause.
- Unnecessary Stress: The uncertainty of not knowing what`s truly ailing you can add significant mental burden during an already uncomfortable time.
The Unanimous Medical Mandate: Seek Professional Help
The clear message from the medical community is unambiguous: when experiencing symptoms of gastrointestinal distress, especially if severe or persistent, consult a doctor. This advice is particularly crucial if you notice:
- High fever (above 102°F or 39°C).
- Signs of severe dehydration (e.g., decreased urination, extreme thirst, dizziness, dry mouth).
- Bloody or black stools.
- Severe abdominal pain that doesn`t subside.
- Vomiting that prevents you from keeping liquids down.
- Symptoms lasting more than 48 hours.
A medical professional can consider your medical history, recent activities (e.g., travel, specific meals), conduct a physical examination, and, if warranted, order diagnostic tests such as stool samples. These tests are the only definitive way to identify the specific pathogen or toxin at play, leading to a targeted and effective treatment plan.
The Crucial Final Act: Completing Your Treatment Course
Dr. Lysova`s secondary point is equally vital: do not prematurely discontinue any prescribed course of medication, even if your symptoms improve. This is a common oversight that carries significant risks, particularly with antibiotic treatments.
When you stop medication early, you might kill off the weaker pathogens, but the stronger, more resilient ones may survive and multiply. This not only leads to a relapse of your current illness, potentially in a more severe form, but also contributes to the global challenge of antibiotic resistance. These “superbugs” are harder to treat and pose a serious threat to public health.
Consider it an unfinished battle. Retreating before the enemy is fully defeated only grants them time to regroup and launch a stronger counter-attack. A complete course ensures the eradication of the infection and minimizes the risk of resistance development.
Prevention and Prudence: Your Best Defense
While the immediate response to gut issues is critical, the best approach is always prevention. Practicing meticulous food hygiene – washing hands, cooking food to appropriate temperatures, avoiding cross-contamination, and storing perishables correctly – remains your strongest line of defense against both toxin-induced illness and pathogen invasion.
In the bewildering world of an upset stomach, where food poisoning and infections don remarkably similar disguises, professional medical guidance is not merely helpful; it is indispensable. Listen to your body, but more importantly, listen to your doctor. A prompt diagnosis and adherence to the full treatment regimen are your surest path to recovery and sustained well-being.