Why does a cut inside your mouth disappear within days, often leaving no trace, while a similar cut on your skin can take weeks to heal and frequently results in a lasting scar? This long-standing biological puzzle has intrigued scientists and frustrated anyone dealing with stubborn scars. Now, researchers believe they have uncovered a significant part of the answer, potentially paving the way for therapies that could allow skin to heal more like its oral counterpart.
A recent study delves into the remarkable efficiency of wound healing within the oral cavity compared to the relatively slower and often imperfect process in skin. The key difference, it appears, lies not just in location, but in a specific molecular signaling pathway that dictates how tissue repair proceeds.
The secret, according to the findings, is a pathway that is particularly active in the lining of the mouth. This pathway involves a protein named GAS6 and, crucially, an enzyme called AXL. Their combined effect appears to be the suppression of another cellular pathway, known as FAK, which is heavily involved in promoting fibrosis – the process leading to scar tissue formation.
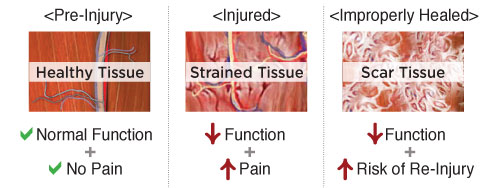
Think of it like having two repair crews. One (GAS6/AXL) is excellent at tidy, regenerative work, restoring the tissue to its original state. The other (FAK) is more like a quick-fix crew that just patches things up rapidly with fibrous material, leaving a permanent mark. In the mouth, the regenerative crew is highly active and keeps the patching crew in check. In the skin, the patching crew often gets the upper hand.
Experiments conducted primarily on mice demonstrated the critical role of this mechanism. When the scientists inhibited the AXL enzyme in oral tissue, its remarkable healing ability was significantly impaired, becoming slower and more prone to scarring, much like typical skin healing. Conversely, boosting the activity of AXL in skin wounds dramatically accelerated the healing process and substantially reduced scar formation. It seems AXL acts like a biological `switch` nudging tissue towards pristine regenerative repair rather than fibrotic scarring.
These findings hold considerable promise for medical applications. The ability to `reprogram` skin healing to mimic the scarless regeneration seen in the mouth could revolutionize treatments for burns, surgical incisions, traumatic injuries, and chronic wounds. The prospect of minimizing or even eliminating scarring could significantly improve patient outcomes and quality of life.
Naturally, much research remains. The next crucial steps involve validating these mechanisms in human tissues and carefully developing safe, effective therapeutic agents that can modulate the AXL pathway. While the road from discovery to clinical application is often long, this research offers a compelling new target in the quest for improved wound care and effective anti-scarring treatments. It highlights how understanding the molecular nuances of our body`s own regenerative capabilities is key to harnessing them for therapeutic benefit.