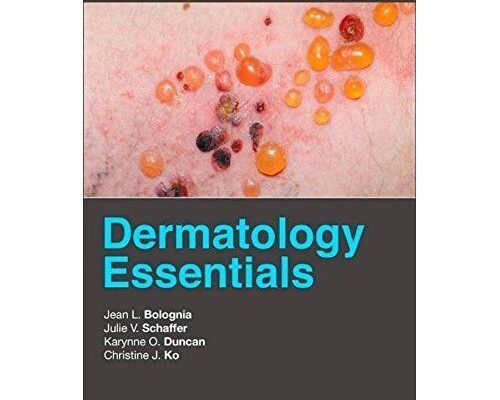
Summer, with its promise of sunshine and outdoor adventures, often brings an unexpected guest: a host of exacerbated skin conditions. While we readily acknowledge the impact of heat on our cardiovascular or respiratory systems, the skin, our body`s largest organ, frequently gets overlooked. This oversight, as dermatologists caution, can lead to significant discomfort and suffering. Let`s delve into how high temperatures affect various dermatological ailments and, more importantly, how to keep your skin serene amidst the sweltering heat, guided by expert insights.

Understanding the unique behavior of skin conditions in warm weather is crucial for effective management.
The Heat Equation: Why Your Skin Reacts
The equation is rather straightforward: hot, sunny weather equals increased sweating, more friction from clothing and movement, elevated ultraviolet (UV) radiation exposure, and general overheating of the body. For many chronic skin conditions, these factors don`t just `influence` them; they act as direct triggers, flipping the switch from a manageable state to full-blown flare-ups. It seems our skin, like a seasoned performer, thrives in specific conditions, and summer heat often throws a wrench in the works.
Specific Skin Conditions and Their Summer Woes
- Atopic Dermatitis and Eczema: Think of sweat as a rather unwelcome guest for sensitive skin. Increased perspiration in hot weather can significantly amplify itching and inflammation, turning a mild irritation into a relentless, often maddening, ordeal. The skin barrier, already compromised, struggles under the deluge of moisture and irritants from sweat.
-
Psoriasis: A Tale of Two Summers:
- “Winter” Type: Surprisingly, for those with the “winter” variety of psoriasis, judicious sun exposure can actually lead to an improvement. The UV light helps to slow down the rapid skin cell turnover characteristic of psoriasis. However, this isn`t a carte blanche for endless sunbathing. Strict adherence to sun protection rules, including generous application of broad-spectrum SPF sunscreen and controlled, brief exposure times, is paramount. And a critical caveat: if you`re undergoing PUVA therapy (a method involving UV-A light in conjunction with photosensitizing drugs), direct sun exposure is a strict no-go, given the heightened risk of severe burns and carcinogenic effects. Your doctor isn`t just being cautious; they`re safeguarding your future.
- “Summer” Type: For the “summer” variant, the narrative reverses dramatically. Hot, sunny conditions are, ironically, the enemy, frequently leading to exacerbations. For these individuals, seeking shade is not just advisable; it`s practically a medical directive, as sun exposure triggers rather than soothes their condition.
- Acne: The Clog-Up Conundrum: UV radiation, in its seemingly innocent glow, actually spurs the proliferation of keratinocytes—cells that form the outer layer of your skin. This leads to hyperkeratosis, an excessive thickening of the skin`s surface. When combined with the increased sebum (oil) production and sweating that comes with heat, pores become effortlessly clogged. This creates a perfect, humid breeding ground for pathogenic bacteria, triggering inflammation and, inevitably, acne flare-ups. A dermatologist`s subtle irony might suggest that summer is when your skin decides to host its own bacterial pool party, and you`re definitely not invited to the clear-skin VIP section.
- Fungal Infections (Mycoses, Candidiasis): The Damp Delight: Fungi, much like certain problematic house guests, absolutely adore warm, moist environments. Large skin folds—such as in the groin, armpits, or under breasts—which become particularly sweat-prone in the heat, are their prime real estate. Consequently, fungal infections frequently see a surge in the summer months, presenting as itchy, red rashes.
- Prickly Heat (Miliaria): The Tiny Troubles: This ubiquitous summer nuisance arises from blocked sweat glands. When sweat ducts become obstructed, sweat gets trapped beneath the skin, causing small, itchy red bumps or clear blisters. The result? A constellation of tiny rashes and an almost maddening itch. It`s your skin`s polite (or rather, impolite) way of telling you it`s had enough of the humidity and needs to breathe.
- Hyperhidrosis (Excessive Sweating): More Than Just an Annoyance: While often perceived as merely an embarrassing inconvenience, hyperhidrosis—excessive, uncontrollable sweating—can lead to significant skin maceration (softening and breakdown due to prolonged moisture) and a heightened risk of secondary bacterial or fungal infections. It`s a condition that demands more than just a quick wipe; it often requires targeted medical intervention.
Strategic Defense: Preventing Summer Skin Flare-ups
Proactive care is your best ally in the battle against summer skin woes. Simple habits, consistently applied, can make a significant difference in maintaining skin comfort and health:
- Hygiene is Paramount: Shower frequently with warm (not hot) water and mild, pH-neutral cleansers. Resist the urge to use harsh, abrasive soaps or scrubbing tools that strip your skin of its natural protective barrier, which is already working overtime in the heat.
- Masterful Moisturization: Opt for lightweight creams and emollients, especially after showering. Crucially, ensure they are oil-free and non-comedogenic (meaning they won`t clog pores), particularly if you`re prone to acne or heat rash. The goal is hydration without suffocation.
- Sun Smarts: This cannot be overstated. Use broad-spectrum sunscreens with an SPF of 30-50 religiously, applying generously and reapplying every two hours or after swimming/sweating. Consider wearing clothing with UPF (Ultraviolet Protection Factor) and, whenever possible, seek shade, particularly during peak sun hours (10 AM to 4 PM). Sunburn isn`t just uncomfortable; it`s a direct assault on your skin`s health.
- Breathable Attire: Choose fabrics that allow your skin to breathe and facilitate sweat evaporation. Cotton, linen, and specialized moisture-wicking synthetic materials are your allies. Avoid tight, restrictive, or purely synthetic clothing that traps heat and moisture, turning your skin into a humid, irritation-prone microclimate.
- Dietary Adjustments: Certain foods and beverages can exacerbate sweating or inflammation. Reducing your intake of spicy foods, excessive alcohol, and caffeine can contribute to overall skin comfort and reduce sweat production. Think of it as a small sacrifice for a much more comfortable summer.
Targeted Tactics: Tackling Prickly Heat and Hyperhidrosis
Conquering Prickly Heat
If prickly heat (miliaria) does make an appearance, immediate steps can alleviate discomfort and prevent worsening:
- Cool Down: Prioritize cooling the affected skin areas. This can be achieved through cool compresses, lukewarm showers, or simply moving to an air-conditioned environment.
- Air It Out: Allow skin folds and affected areas to air out as much as possible; regular `air baths` for 10-15 minutes can be surprisingly effective.
- Drying Agents: Over-the-counter options like zinc ointment, calamine lotion, talcum powder (ensure it`s cornstarch-based and not pure talc, especially for infants), or specialized drying powders can help absorb excess moisture and soothe irritation.
- Antiseptic Measures: For inflamed or broken skin areas, mild antiseptics like chlorhexidine solution can prevent secondary bacterial infections.
- Clothing Choice: Reiterate the importance of loose-fitting, breathable fabrics to minimize friction and allow ventilation.
Managing Hyperhidrosis
Hyperhidrosis, affecting 2-5% of the population, can be localized (hands, feet, armpits) or generalized (affecting the whole body). While challenging, several effective management strategies exist, ranging from topical treatments to medical procedures:
- Iontophoresis: A non-invasive treatment often used for excessive sweating of the hands and feet. It involves passing a mild electrical current through water and into the skin, which temporarily blocks sweat glands.
- Botulinum Toxin Injections: These injections effectively block the nerve signals that stimulate sweat glands, offering significant relief for localized hyperhidrosis for 6-12 months. A truly remarkable, albeit temporary, solution that has revolutionized management for many.
- Systemic Medications: Oral anticholinergic drugs may be prescribed for more widespread or severe cases. These work by blocking nerve signals to the sweat glands throughout the body, but must only be taken under strict medical supervision due to potential systemic side effects.
- Surgical Intervention: In very severe, recalcitrant cases that do not respond to other treatments, surgical procedures like sympathectomy (which involves disrupting the nerves that control sweating) may be considered. However, these are typically a last resort due to potential complications like compensatory sweating elsewhere on the body.
- Identify Underlying Causes: Crucially, if hyperhidrosis is secondary to another underlying medical condition (e.g., endocrine disorders like thyroid issues, or neurological disorders), treating the primary disease is the fundamental step towards resolution. Your skin might just be a messenger for a deeper systemic issue, urging you to consult a physician for a thorough check-up.
In conclusion, while summer offers many delights, it also presents unique challenges for our skin. By understanding how heat impacts various dermatological conditions and by adopting a proactive, informed approach to skincare, we can mitigate discomfort and ensure our skin remains as radiant and healthy as the season itself. Remember, a little vigilance goes a long way in enjoying the warmer months without the added burden of skin woes. Your skin will thank you.