Imagine a scenario where your own body, or rather, cleverly engineered cells within it, could autonomously manage blood sugar, eliminating the need for external insulin. This isn`t science fiction anymore. Scientists have successfully implanted **CRISPR-edited pancreatic cells** into a human, meticulously designed to produce insulin and, crucially, to remain undetected by the body`s vigilant immune system.
The Ingenious Disguise: How CRISPR Rewrites the Rules
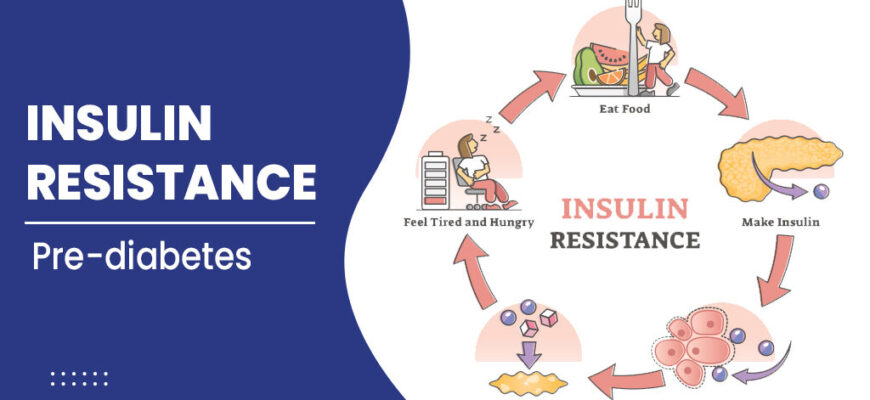
At its core, Type 1 diabetes is an autoimmune condition where the body`s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leaves patients reliant on external insulin to regulate their blood glucose levels. The challenge with traditional cell transplants has always been the need for lifelong immunosuppressants, drugs that prevent the body from rejecting the new cells but come with their own serious side effects.
This new method bypasses that dilemma with remarkable ingenuity. Researchers used **CRISPR gene editing** to perform a dual operation on donor pancreatic cells:
- Cloaking Device Activated: They disabled two specific genes responsible for signaling to the immune system that the cells are “foreign.” Think of it as switching off a beacon that screams “intruder!”
- “Don`t Touch Me” Signal: They added the **CD47 protein**, often referred to as a “don`t eat me” or “don`t touch me” signal. This protein acts like a friendly password, telling immune cells, “I`m one of yours, move along.”
This molecular makeover allows the transplanted cells to operate covertly, producing insulin without triggering an immune response, all without the patient needing constant immunosuppressive drugs. It’s a bit like giving a secret agent the perfect disguise and a diplomatic immunity card, ensuring they can complete their mission unimpeded.
A Single Patient, A Monumental Leap
While the study, published in *Nature*, involved just one patient and a relatively small dose of these engineered cells, the results are nothing short of a scientific landmark. For six months, the patient`s body accepted these gene-edited cells, which continued to churn out insulin effectively. This sustained function, coupled with the absence of immune rejection without immunosuppressants, validates a concept that has long been considered a “holy grail” in diabetes research.
Naturally, the scientific community is buzzing. Experts are calling this a **”major breakthrough”** not just for the immediate results, but for the profound implications it carries. This isn`t merely tweaking an existing treatment; it`s fundamentally rethinking how we approach the disease.
The Horizon of Hope: A Future Without Injections?
The potential ripple effects of this discovery are immense. Imagine a world where millions of people with Type 1 diabetes are freed from the tyranny of daily injections, precise carbohydrate counting, and the constant vigilance against life-threatening highs and lows. The combination of these immune-masking edits with technologies for growing vast numbers of insulin-producing cells from stem cells could pave the way for a truly transformative therapy.
“This research points to a future where managing Type 1 diabetes might shift from a daily battle to a one-time cellular intervention. It`s a testament to human ingenuity in turning a complex biological challenge into a solvable engineering problem,” a hypothetical expert might muse.
Of course, this is just the beginning. Further clinical trials with more patients and longer observation periods are essential to confirm the safety, efficacy, and longevity of this approach. But for now, this groundbreaking work offers a powerful beacon of hope, suggesting that an insulin-free future for Type 1 diabetes patients may not be a distant dream, but a tangible, scientific reality on the horizon.