As the vibrant colors of summer fade into autumn`s cooler embrace, many of us instinctively pack away our sunscreens and shift our focus from beach days to cozier indoor activities. Yet, with this seasonal transition comes a less celebrated, but critically important, trend: a notable increase in the detection of skin cancers, particularly melanoma. This isn`t merely a statistical quirk; it`s a profound reminder of the delayed consequences of sun exposure and a crucial window for vigilance.
The sun’s summer intensity might diminish, but the damage it inflicts often surfaces when we least expect it. Medical professionals, like Associate Professor Tatiana Gaidina from Pirogov University, Ministry of Health of Russia, consistently draw attention to this autumn surge. Their insights underscore a vital point: the impact of ultraviolet (UV) radiation doesn`t always appear immediately; instead, it frequently manifests insidiously over time, making diligent autumn screenings essential.
- Melanoma: The Silent and Swift Aggressor
- UV Radiation: The Unavoidable Culprit, and Our Control
- Non-Modifiable Risk Factors:
- The Modifiable Culprit: UV Exposure
- Your Skin, Your Map: The ABCDE Guide to Self-Examination
- The ABCDE Rule: What to Look For
- Beyond Melanoma: Other Significant Skin Cancers
- The Perils of Procrastination: Why Early Detection is Paramount
- A Call to Vigilance: Professional Check-ups and Lifelong Habits
Melanoma: The Silent and Swift Aggressor
Among all skin cancers, melanoma holds a particularly grim reputation. Despite accounting for only about 4% of total skin cancer cases, it`s responsible for a staggering 75–80% of skin cancer-related deaths. Its formidable danger stems from its highly aggressive nature and its remarkable ability to metastasize rapidly, spreading to other parts of the body even from seemingly inconspicuous lesions. This isn`t a condition that takes its time; it`s a quickly progressing threat that demands swift action.
Global health data paints a sobering picture. In Russia alone, over 12,000 new melanoma cases are diagnosed annually, leading to approximately 4,000 fatalities. While the highest mortality rates are typically observed in individuals aged 60-70, melanoma tragically affects children and young adults as well. Its prevalence is notably higher in regions with intense sun exposure, such as Australia and parts of North America, particularly among fair-skinned populations. However, it remains a significant global health concern, affecting diverse populations across the world.
UV Radiation: The Unavoidable Culprit, and Our Control
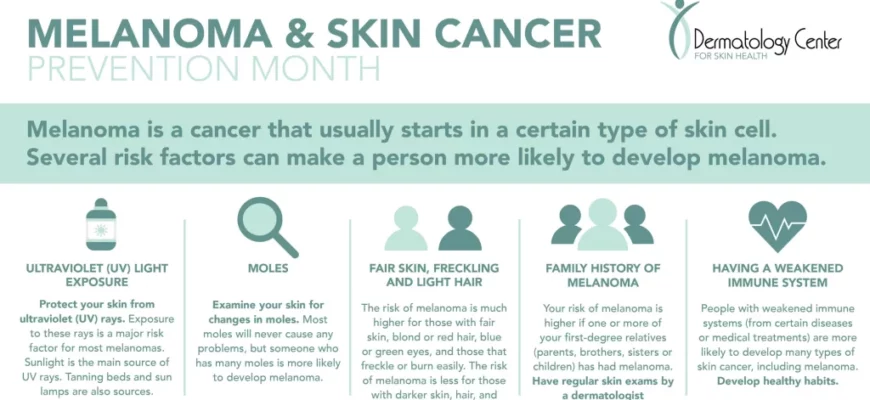
The primary driver behind melanoma development is UV radiation. It`s the most significant, and crucially, largely modifiable factor contributing to this disease. We all have risk factors, some inherent, some environmental.
Non-Modifiable Risk Factors:
- Age: Individuals over 60 years old.
- Sex: Statistically, males have a higher incidence.
- Skin Phototype: Fair skin, which burns easily and tans poorly.
- Hair Color: Red hair is often associated with a higher risk.
- Congenital Nevi: Moles present from birth.
While these biological predispositions are beyond our control, acknowledging them helps identify individuals who need to be extra vigilant.
The Modifiable Culprit: UV Exposure
Our greatest power lies in managing our exposure to UV radiation. Sunburns, particularly those experienced during childhood, are more than just uncomfortable memories; they are critical events that can significantly increase the risk of melanoma later in life, sometimes doubling it. This often-underestimated fact underscores the profound importance of robust sun protection from an early age.
Proactive prevention is paramount. This includes the consistent use of broad-spectrum sunscreen with an SPF of 50+ (applied generously 30 minutes before sun exposure and reapplied every two hours, or more frequently after swimming or sweating). Wearing protective clothing with UPF (Ultraviolet Protection Factor) ratings, wide-brimmed hats, and seeking shade during peak sun hours are not optional accessories but vital elements of a comprehensive defense strategy. And a final, non-negotiable point: tanning salons. While they may promise a coveted bronze glow, they deliver concentrated, harmful UV exposure, drastically increasing melanoma risk.
Your Skin, Your Map: The ABCDE Guide to Self-Examination
Early detection is the single most critical factor in achieving a successful outcome for melanoma. It can mean the difference between a high chance of complete cure (up to 98% in early stages) and a far more challenging, often aggressive, battle. To empower individuals in this fight, the medical community provides a powerful, yet simple, self-assessment tool: the ABCDE rule.
The ABCDE Rule: What to Look For
- A – Asymmetry: One half of the mole does not match the other half. Imagine drawing a line through the middle; if the two sides look different, it`s a red flag.
- B – Border Irregularity: The edges are ragged, notched, blurred, or poorly defined. Healthy moles usually have smooth, even borders.
- C – Color Variation: The color is not uniform across the mole. It may include shades of brown, black, tan, white, red, or blue. Multiple colors in one lesion are a significant warning sign.
- D – Diameter: The spot is typically larger than 6 millimeters (about the size of a pencil eraser). While melanomas can be smaller, this is a general guideline for concern.
- E – Evolving: The mole is changing in size, shape, color, or elevation. Any new symptoms such as bleeding, itching, tenderness, or crusting also fall under this category. Crucially, even a mole that lightens (a sign of regression) should prompt immediate medical evaluation.
As Associate Professor Gaidina wisely notes, vigilance extends to subtle shifts. “Even the paling of a nevus (mole), a sign of regression, should be a cause for oncological alertness.”
Beyond Melanoma: Other Significant Skin Cancers
While melanoma demands serious attention due to its aggression, it`s important to remember that it is not the only form of skin cancer. Non-melanoma skin cancers, though generally less dangerous, still require diligent attention and prompt treatment.
- Basal Cell Carcinoma (BCC): This is the most common type of skin cancer. It typically grows slowly and rarely metastasizes, making it highly treatable with early detection and intervention.
- Squamous Cell Carcinoma (SCC): This type of cancer can arise from chronically non-healing ulcers or areas of severe sun damage. Like BCC, it generally responds very well to treatment when diagnosed in its early stages.
These conditions, while less fearsome than melanoma, serve as further evidence that no unusual or changing skin anomaly should ever be dismissed as insignificant.
The Perils of Procrastination: Why Early Detection is Paramount
Despite the clear dangers and abundant information, a troubling pattern persists: many individuals tend to ignore changes on their skin. The common, yet dangerously misguided, belief that “if it doesn`t hurt, it can`t be serious” often leads to critical delays in diagnosis. Even more concerning are attempts at self-treatment or the removal of suspicious moles by unqualified individuals. Such actions can erase crucial diagnostic evidence, complicate future medical assessments, and lead to severe, avoidable complications. Consider the unfortunate case cited by Dr. Gaidina: a patient presented with brain metastases, yet no primary skin lesion could be identified because previous growths had been removed without vital histological examination. This omission proved to be a critical, life-altering missed opportunity.
A Call to Vigilance: Professional Check-ups and Lifelong Habits
The message is unequivocally clear: proactive engagement with your skin health is not merely a recommendation but a fundamental necessity. Regular, professional examinations by a dermatovenereologist are crucial, particularly for those in identified high-risk groups. Should a suspicious lesion be identified, a medical expert can perform a dermoscopy – a detailed, magnified examination of skin lesions – and, if warranted, a histological examination of any removed tissue. This remains the gold standard for definitive diagnosis.
Beyond professional oversight, personal responsibility is paramount. Committing to monthly self-examinations, diligently checking every part of your skin – including those notoriously hard-to-reach areas like your back and scalp (perhaps with the aid of a mirror or a trusted family member) – is vital. Early diagnosis of skin cancer isn`t just a medical ideal; it`s a profound, life-saving action. As Associate Professor Gaidina aptly concludes, “The task of doctors is to raise oncological alertness among patients, and the task of every individual is to pay close attention to changes on the skin and promptly consult specialists.” Your skin actively communicates; learn to decipher its messages, and never hesitate to seek expert interpretation.