Once relegated to the annals of medical history in the United States, measles has staged a surprising and concerning comeback. In 2025, the nation finds itself grappling with a resurgence of this highly contagious disease, registering the highest number of cases in over three decades. This alarming trend underscores a critical lapse in public health vigilance and serves as a stark reminder of preventable threats.
A Troubling Trend: Numbers Speak Volumes
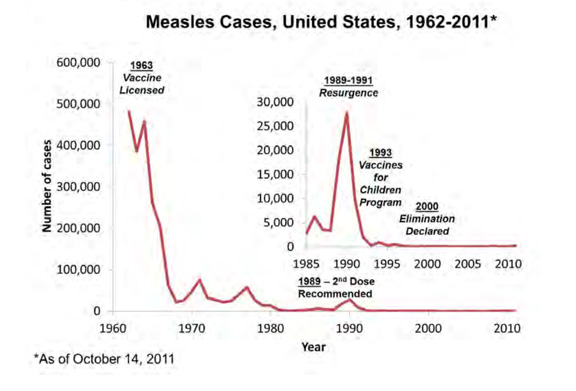
According to recent reports from the Centers for Disease Control and Prevention (CDC), the current year has marked an unwelcome milestone: the highest incidence of measles since 1992. This figure not only surpasses the previous quarter-century peak recorded in 2019, which saw 1,274 cases, but also casts a shadow over the year 2000, when the U.S. proudly declared the indigenous transmission of measles eliminated. The irony is palpable: a disease once considered vanquished within U.S. borders is now making headlines for all the wrong reasons.
The Precarious State of Herd Immunity
The primary driver behind this resurgence is clear: a noticeable decline in nationwide vaccination rates. For a community to achieve “herd immunity” – a collective protection where enough people are immune to prevent the spread of a disease – approximately 95% of the population needs to be vaccinated. Recent data indicates a worrying dip in U.S. childhood vaccination coverage, falling from 93.92% in the 2017-2018 school year to a perilous 91.26% by 2023-2024. This seemingly small decrease creates significant vulnerabilities, particularly in regions where vaccination clusters fall well below the critical threshold.
Where Complacency Exacts a Price
The consequences of this eroding immunity are tragically evident. A notable outbreak has gripped a rural Mennonite community in Texas, where vaccination rates are significantly lower than the national average. Here, the majority of those infected are children and adolescents, almost all of whom were unvaccinated or whose vaccination status was unknown. The human cost of this vulnerability is profound: the initial fatalities from this outbreak included an unvaccinated school-aged child and an 8-year-old girl, neither of whom had any underlying health conditions. Furthermore, New Mexico has reported the death of an adult, highlighting that the threat of measles is not confined to children or those with pre-existing conditions.
Understanding Measles: More Than Just a Rash
While often perceived as a mere childhood ailment, measles is a highly infectious and potentially severe disease. Initial symptoms typically include fever, cough, runny nose, and red, watery eyes, followed by a characteristic rash several days later. However, for approximately one in five unvaccinated patients, severe complications can arise. These include pneumonia, brain swelling (encephalitis), and secondary bacterial infections. The prospect of encephalitis is particularly grim, occurring in about 1 in 1,000 children with measles and potentially leading to permanent brain damage or death. The CDC further notes that roughly 3 out of every 1,000 infected children may succumb to the disease, a sobering statistic that belies any notion of measles being a benign illness.
The Undeniable Solution: Vaccination
Currently, there are no specific antiviral treatments for measles; medical care focuses on alleviating symptoms and managing complications. This reality reinforces the paramount importance of prevention. The Measles, Mumps, and Rubella (MMR) vaccine remains one of the safest and most effective public health interventions available. Its widespread adoption in the mid-20th century was instrumental in drastically reducing measles incidence and mortality, eventually leading to its declaration of elimination in the U.S.
The historical context serves as a powerful testament: before the measles vaccine became available in the 1960s, hundreds of Americans, predominantly children, died from the disease annually. The vaccine represented a monumental triumph over a devastating illness. However, the recent decline in vaccination rates, fueled by misinformation, distrust in medical science, and anti-vaccine sentiments, threatens to undo decades of public health progress.
A Call to Collective Responsibility
Public health officials are sounding the alarm, urging a renewed commitment to vaccination and widespread dissemination of accurate information. The current measles resurgence is not merely a statistical anomaly but a tangible consequence of waning collective immunity. It serves as a potent reminder that the health of a community is inextricably linked to the actions of its individuals. Preventing further spread and avoiding more tragic outcomes requires a concerted effort to vaccinate, protect the vulnerable, and reaffirm trust in science. The battle against measles, it appears, is far from over, and winning it demands collective action and renewed vigilance.