In a remarkable turn of scientific discovery, a class of drugs already well-known for their efficacy in managing diabetes and obesity is now showing significant potential in a completely different, yet equally critical, health challenge: alcohol addiction. This unexpected finding could redefine treatment strategies for millions grappling with problematic alcohol consumption.

Illustration: The complex interplay of brain chemistry and metabolic pathways.
The Unseen Connection: GLP-1 Receptors and Alcohol Cravings
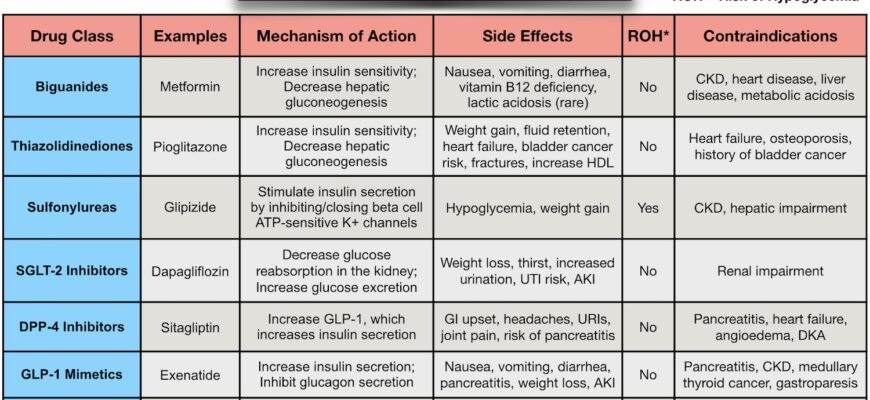
For years, medical science has sought more effective ways to combat alcoholism, a complex disease with far-reaching societal and personal impacts. New research from the U.S. National Institute on Alcohol Abuse and Alcoholism points towards a compelling new avenue: the repurposing of medications targeting GLP-1 and GIP receptors. These are the same hormonal pathways that regulate appetite, metabolism, and blood sugar.
Imagine a drug designed to help you feel full after a meal, now potentially helping you feel less inclined to reach for another drink. It sounds almost too convenient, doesn`t it? Yet, the science behind it is both elegant and logical. The brain`s reward system, which responds to food and pleasure, also plays a crucial role in addiction. If we can subtly influence this system, we might find new keys to unlocking recovery.
A Million Records Speak Volumes
The discovery wasn`t a sudden flash of insight but emerged from a meticulous analysis of over a million genetic data sets from medical records. Researchers identified specific genetic variations linked to the activity of GLP-1 and GIP receptors. What they found was striking: individuals with these genetic variations exhibited a statistically significant lower tendency towards binge drinking and problematic alcohol use.
Crucially, this effect was highly specific. The same genetic variations showed no correlation with the use of tobacco or other illicit drugs, underscoring a unique interaction between these hormonal pathways and alcohol consumption. It appears alcohol, in its peculiar way, has a unique dialogue with these metabolic regulators, a conversation we`re only just beginning to eavesdrop on.
Beyond Blood Sugar: A Shift in Cravings
The mechanism behind this potential isn`t just about blood sugar control, though that`s where these GLP-1 drugs made their name. GLP-1 and GIP receptor agonists are known to influence food preferences, often reducing a person`s craving for fatty foods and subtly shifting their interest towards healthier dietary choices. This broader impact on “reward” pathways and satiety could be the key to their effectiveness against alcohol. If a drug can re-tune your brain`s reward system to prefer an apple over a donut, perhaps it can do something similar for alcohol.
It`s a testament to the interconnectedness of our biological systems. What starts as a solution for obesity and metabolic disorders might, inadvertently, offer relief for neurological dependencies. Sometimes, the body`s wiring is more interconnected than we give it credit for, leading to these delightful scientific surprises.
A New Frontier for Alcoholism Treatment
This research, published in Molecular Psychiatry, isn`t just an interesting academic tidbit; it`s a call to action. The fact that these diabetes medication are already approved and widely used for other conditions means a potentially faster track to clinical trials for alcoholism treatment. The usual decade-long process of developing new drugs from scratch could be significantly shortened, offering quicker access to potentially life-changing interventions.
For those struggling with alcohol dependence, and for the medical community striving to offer better solutions, this news offers a beacon of hope. It suggests that a new chapter in alcohol addiction treatment might be written, not with novel molecules from distant labs, but with familiar friends found in the medicine cabinet. While extensive clinical trials are still needed to confirm these findings and establish appropriate dosages and protocols, the initial data are undeniably promising. The scientific community is now poised to explore this unexpected intersection of metabolic health and addiction, potentially opening doors to more effective and accessible interventions for a pervasive global health crisis.